
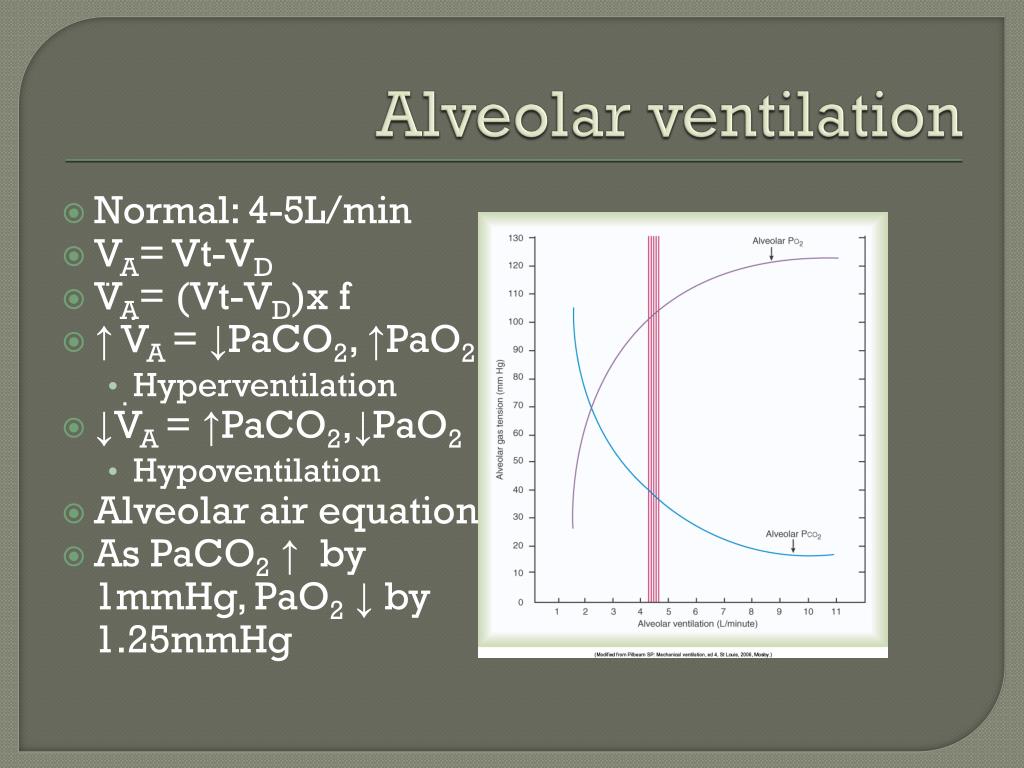
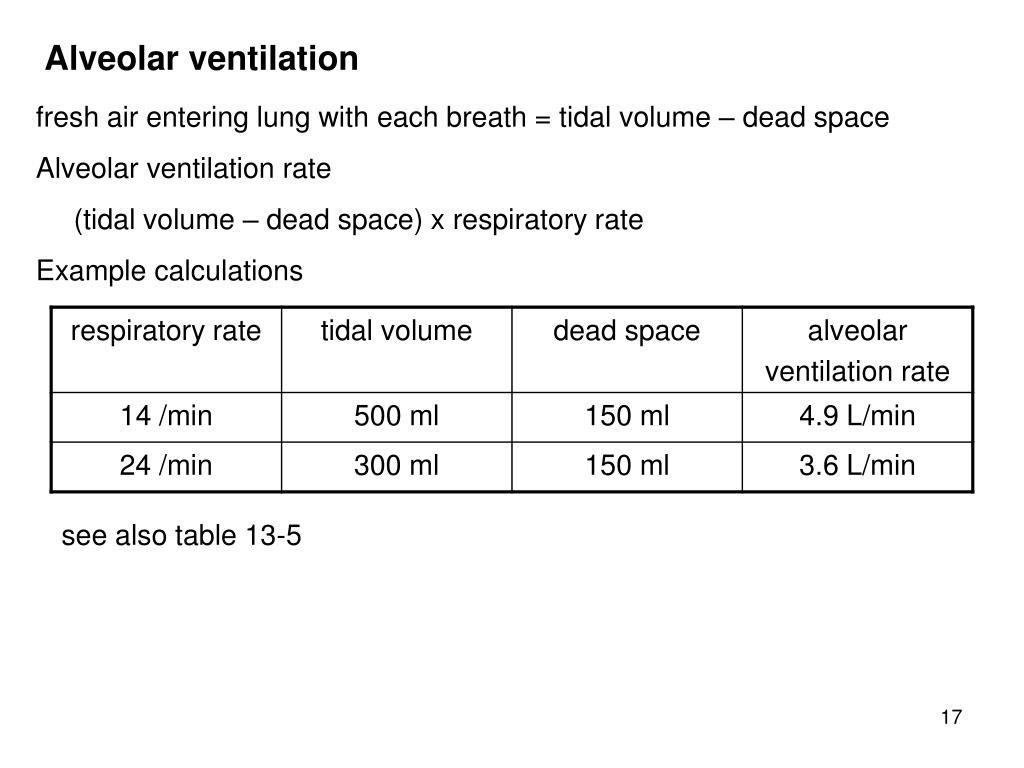
RESUMEN INTRODUCCIÓN: Durante la actual pandemia de COVID-19 ha surgido la preocupación sobre el posible riesgo de que la ventilación no invasiva (VNI) promueva la transmisión aérea. Re-evaluation of treatment efficiency and settings is crucial whenever protective measures influencing NIV equipment are considered. CONCLUSIONS: Modifications of NIV configurations in the context of COVID-19 pandemic result in substantial increase of instrumental dead space. Compared to reference, all the configurations evaluated required substantial increase in VTE to preserve alveolar ventilation, ranging from +79(2) to +216(1) mL. RESULTS: Reference PETCO2 was 38(0) mmHg, with a PS set at 10 cmH2O, resulting in a VTE of 432(2) mL. Resulting VTE was recorded as primary outcome. For each configuration, pressure support (PS) was gradually increased to reach reference PETCO2. Then, five different circuit configurations including non-vented facial mask with viral/bacterial filter, modification of leak position, and change from single to double- limb circuit were evaluated. The model was ventilated through usual domiciliary configuration (single limb circuit with facial vented mask) which was used as reference. METHODS: A bench consisting of a test lung connected to an adult-sized mannequin head was set up. We therefore designed this study to evaluate their effects on the tidal volume (VTE) required to preserve stable end-tidal CO2 partial pressure (PETCO2) with constant respiratory rate. However, all these configurations increase instrumental dead space.
In case of hospital admission, continuation of therapy in patients undergoing chronic NIV is necessary and several protective circuit configurations have been recommended to reduce the risk of aerosol dissemination.

ABSTRACT INTRODUCTION: With the current COVID-19 pandemic, concerns have raised regarding the risk for NIV to promote airborne transmission.


 0 kommentar(er)
0 kommentar(er)
